
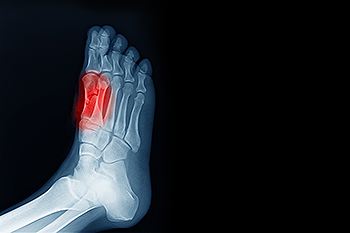
The group of bones that are under the bottom of the big toe include the sesamoid bones. They protect specific tendons in the foot, and absorb most of the weight on the inside of the foot. The condition that is known as sesamoiditis occurs when the sesamoid bones become inflamed. They can become injured as a result of enduring a stress fracture, or from an injury that comes from repetitive motion consisting of dancing. Many patients need to have a proper diagnosis performed, which includes having an X-ray taken that can rule out a fracture. Correct treatment techniques can possibly reduce painful symptoms, in addition to protecting the foot from further injury. These can consist of wearing orthotic insoles, taking anti-inflammatory medication, or possible surgery. If you feel you have injured your sesamoid bones, it is strongly urged that you confer with a podiatrist who can help you to manage this condition, in addition to offering you correct treatment solutions.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact the podiatrists of The Foot & Ankle Center of New Jersey. Our doctors will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Paramus, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis is a condition that affects the joint that is just behind the big toe in the area known as the ball of the foot. It is most common in younger people and people who have just begun an exercise program. Since the sesamoid bones are like a pulley controlling the big toe, they can rub against each other and cause a gradual onset of pain. Pain may also be caused by the inflammation of tendons surrounding the bones. If ignored, sesamoiditis can lead to other, more serious problems such as severe irritation and fractures of the bones.
The cause of sesamoiditis is sudden increase in activity. The ball of your foot acts as a springboard to help you lift off when you are jogging or running. Sudden increase in the use of these bones or the tendon that controls them can cause irritation. The tendon then begins to develop inflammation and the joint begins to swell. People with smaller, bonier feet or those with a high arch are typically more susceptible to this condition.
Sesamoiditis is fairly simple to diagnose since the symptoms have a gradual onset rather than a sudden impact. The symptoms begin with slight irritation around the joint shortly after the increase in activity. The discomfort eventually turns to pain with light swelling and possibly redness. Although redness or bruising are rare, this may be a symptom. After each session of exercising, the aggravated joint becomes more irritated and increases into a very intense throbbing.
Treatment for sesamoiditis can vary depending on the severity of the situation. However, treatment is almost always approached in a noninvasive way. For a case that is just beginning the doctor may recommend a very strict rest period that will limit the activity allowed on the joint. If you must be active, a recommendation for as modified shoe or insole, along with bandaging and immobilizing the big toe will be made to ensure that pressure is not placed on the joint. For severe cases, it is typically recommended that the joint and the big toe be completely immobilized to allow adequate time to heal. Ice and an over the counter anti-inflammatory may can help with the pain and discomfort while you are at rest.
When you return to your regular exercise activities, it is recommended that you use an insole that will allow even distribution of impact to your entire foot, rather than just the balls of your foot. This will prevent further aggravation of the injury.

When body tissue is exposed to the environment, it is known as an open wound. Proper wound care is needed if there is bleeding, or if you have developed a broken bone. A closed wound occurs when there is bleeding under the surface of the skin and is referred to as a bruise. A break in the skin that comes from a fall or surgery is an open wound and requires immediate medical attention. The first step would be to stop the bleeding, followed by cleaning the wound. If the wound is severe antibiotics may be needed, and the wound can be dressed. It is important to change the dressing routinely, and this helps check if an infection has developed. Many diabetic patients are prone to developing wounds on the feet, and proper treatment must be provided. If you have a wound on your foot, it is suggested that you consult with a podiatrist who can offer you the best remedy for wound care on the feet.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with the podiatrists from The Foot & Ankle Center of New Jersey. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Paramus, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
If you have heel pain and think you might have plantar fasciitis, assess your risk factors. Do you stand for prolonged periods of time or run excessively? Do you lead a sedentary lifestyle or have a body mass index (BMI) greater than 27? Do you pronate (turn your foot inward) excessively when you walk? Do you have high arches? Is it difficult for you to bend your ankle? Now, contemplate the pain you are experiencing. Does it feel worse when you first get out of bed in the morning, then get better after you start to move around, only to return towards the end of the day? If you answered yes to one or more of these questions, you are at an increased risk of developing plantar fasciitis and are exhibiting its typical symptoms. Plantar fasciitis occurs when the connective plantar fascia tissue on the sole of the feet becomes damaged/torn and irritated. A podiatrist can make an accurate diagnosis of this most common form of heel pain and use a variety of treatments to heal the plantar fascia and relieve your pain.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact the podiatrists from The Foot & Ankle Center of New Jersey. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Paramus, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
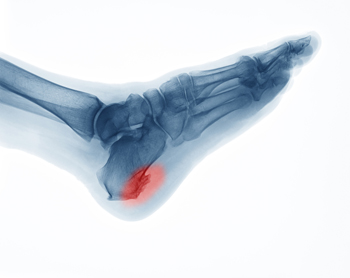 Heel spurs, or “enthesophytes,” develop on the heel of the foot. There are two types of heel spurs associated with different heel problems. One type of heel spur is called a Plantar Spur. It is linked to a problem called “Heel Spur Syndrome” and is a bone spur that develops on the bottom of the heel, on the sole of the foot where the plantar fascia (a band of fibrous tissue that stretches along the bottom of the foot) connects to the heel bone. People who have plantar fasciitis are prone to developing these kinds of spurs, which are the bone’s response to stress from straining foot muscles and ligaments, overstretching the plantar fascia, or repeated tearing of the thin lining of the heel bone. They are also associated with age, obesity, and osteoarthritis. Heel spurs are less likely to feel painful. The other type of heel spur is a Dorsal Spur and is connected to a problem called “Insertional Achilles Tendonitis,” a condition where a bone spur develops at the back of the heel, where the Achilles tendon fits into the bone. If you notice a bony protrusion on the heel of your foot or have pain in this area, it is best to consult with a podiatrist who can diagnose the problem and recommend proper treatment.
Heel spurs, or “enthesophytes,” develop on the heel of the foot. There are two types of heel spurs associated with different heel problems. One type of heel spur is called a Plantar Spur. It is linked to a problem called “Heel Spur Syndrome” and is a bone spur that develops on the bottom of the heel, on the sole of the foot where the plantar fascia (a band of fibrous tissue that stretches along the bottom of the foot) connects to the heel bone. People who have plantar fasciitis are prone to developing these kinds of spurs, which are the bone’s response to stress from straining foot muscles and ligaments, overstretching the plantar fascia, or repeated tearing of the thin lining of the heel bone. They are also associated with age, obesity, and osteoarthritis. Heel spurs are less likely to feel painful. The other type of heel spur is a Dorsal Spur and is connected to a problem called “Insertional Achilles Tendonitis,” a condition where a bone spur develops at the back of the heel, where the Achilles tendon fits into the bone. If you notice a bony protrusion on the heel of your foot or have pain in this area, it is best to consult with a podiatrist who can diagnose the problem and recommend proper treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact the podiatrists from The Foot & Ankle Center of New Jersey. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Paramus, NJ . We offer the latest in diagnostic and treatment technology to meet your needs.